Impact of Endotracheal Tube Exchange on Lung Health in Preterm Infants with Chronic Lung Disease
Endotracheal intubation remains a cornerstone of respiratory support for preterm infants suffering from chronic lung disease (CLD)—a condition marked by ongoing respiratory insufficiency after premature birth. However, the risks and benefits of endotracheal tube (ETT) exchange in these fragile patients have been a matter of clinical debate. A recent study published in the Journal of Perinatology offers a comprehensive examination of the safety, procedural risks, and effects on pulmonary mechanics associated with ETT exchange in preterm infants with CLD. The findings provide valuable insights that can refine neonatal airway management and promote evidence-based care.
The study centers on a key challenge in neonatal intensive care: deciding whether and when to replace a malfunctioning or malpositioned ETT in infants with delicate lungs. While tube exchange can be necessary to restore proper ventilation, quantitative data on its physiological impact have been limited. By evaluating a cohort of preterm infants who underwent tube exchange, the researchers meticulously assessed peri-procedural stability, adverse event rates, and post-procedural changes in lung mechanics such as compliance, resistance, and tidal volume.

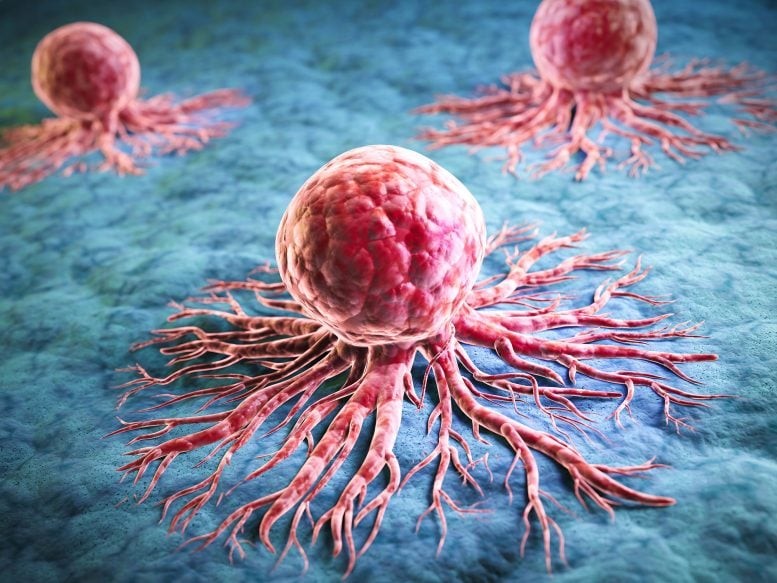
Figure 1. Infants with Chronic Lung Disease.
Using advanced monitoring tools adapted for neonatal care, the study captured precise, real-time data before and after tube replacement—offering a clearer picture than previous anecdotal reports. The results revealed that, under strict procedural standards and expert handling, ETT exchange was generally safe, showing no statistically significant rise in complications like hypoxia, bradycardia, or accidental extubation. This supports a cautious but confident approach to tube replacement when clinically warranted. Figure 1 shows Infants with Chronic Lung Disease.
Beyond procedural safety, the study identified temporary declines in lung compliance immediately after tube exchange, likely due to brief disruptions in alveolar stability or surfactant distribution. Encouragingly, these changes were short-lived, with lung function returning toward baseline within hours, demonstrating both the vulnerability and resilience of the premature lung.
Importantly, the research underscored the critical role of tube size optimization. Infants who received a properly sized or slightly larger tube during exchange exhibited improved tidal volumes and compliance, while those retaining smaller tubes showed less favorable outcomes. This finding reinforces the importance of individualized tube selection based on evolving pulmonary needs.
Timing also proved significant—earlier intervention for suspected tube dysfunction was associated with better outcomes, likely by preserving ventilation stability and preventing secondary lung injury [1]. Delayed exchanges, in contrast, risked exacerbating inflammation and mechanical trauma.
The study further emphasized the need for ventilator readjustment after tube replacement. Because even transient changes in airway resistance and compliance can affect gas exchange, clinicians are advised to re-evaluate ventilator settings such as PEEP, inspiratory pressure, and timing immediately following the procedure.
Additionally, the authors called for enhanced training and standardization in neonatal airway management. Variations in operator skill and technique can impact both safety and respiratory outcomes, highlighting the value of simulation-based training and multidisciplinary collaboration.
Looking ahead, the study points toward technological innovations—such as sensor-equipped tubes to monitor position and patency in real time—that could minimize the need for unnecessary exchanges. It also advocates exploring less invasive exchange techniques to further reduce procedural stress.
Beyond neonatology, these findings enrich broader critical care knowledge by illustrating how airway interventions influence lung mechanics in vulnerable patients. The research balances procedural necessity with ethical responsibility, advocating for transparent, family-centered communication and evidence-based decision-making.
Future work should examine the long-term effects of repeated tube exchanges on lung development and function, potentially guiding preventive strategies for chronic respiratory morbidity. Integrating real-time pulmonary mechanics monitoring into standard NICU protocols could enhance both safety and individualized care.
In essence, this landmark study advances neonatal respiratory medicine by bridging crucial gaps in understanding. It demonstrates that, with precision, expertise, and monitoring, endotracheal tube exchange can be performed safely in preterm infants while minimizing adverse effects on fragile lungs. Ultimately, these insights empower clinicians to make informed decisions—protecting pulmonary function today while supporting healthier outcomes for the most vulnerable patients of tomorrow.
References
- https://bioengineer.org/endotracheal-tube-exchange-impacts-in-preterm-lung-disease/
Cite this article:
Keerthana S (2025), Impact of Endotracheal Tube Exchange on Lung Health in Preterm Infants with Chronic Lung Disease, AnaTechMaz, pp.515